General Information
The gastrointestinal (GI) tract is part of the digestive system, which processes nutrients in foods that are eaten and helps pass waste material out of the body. The GI tract includes the stomach and intestines (bowels).
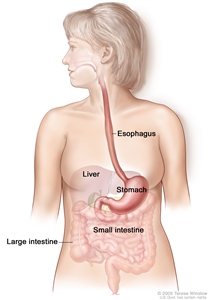
The esophagus and stomach are part of the upper gastrointestinal (digestive) system.
- Food moves from the throat to the stomach through a tube called the esophagus.
- After food enters the stomach, it is broken down by stomach muscles that mix the food and liquid with digestive juices.
- After leaving the stomach, partly digested food passes into the small intestine and then into the large intestine.
- The end of the large intestine, called the rectum, stores the waste from the digested food until it is pushed out of the anus during a bowel movement.
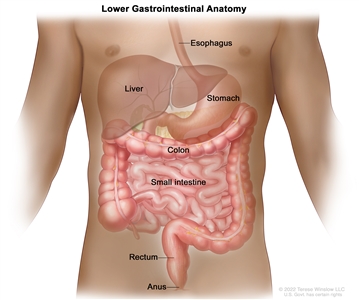
Anatomy of the lower gastrointestinal (digestive) system showing the colon, rectum, and anus. Other organs that make up the digestive system are also shown.
GI complications refer to a range of problems that can affect the digestive system. GI complications are common in people with cancer and may be caused by the cancer itself, or it can be an effect of cancer treatment or the medicines used to manage symptoms.
Children and adults with cancer may experience similar types of GI complications, but the causes and treatment approaches differ based on age and other factors. This page describes the following GI complications in adults, their causes, and treatments:
- constipation
- fecal impaction
- bowel obstruction
- diarrhea
- radiation enteritis
Constipation
Constipation is a condition in which bowel movements are difficult or painful to pass and don't happen very often.
Constipation is caused by the slow movement of stool through the large intestine. As the stool slowly moves through the large intestine, it loses fluid and becomes harder.
A person with constipation may be unable to have a bowel movement, have to push harder to have a bowel movement, or have infrequent bowel movements.
There is no "normal" number of bowel movements for a person with cancer. Each person is different. However, if you have infrequent bowel movements, you may be constipated.
Constipation is a common problem for people with cancer.
Common causes of constipation include older age, changes in diet and fluid intake, and not getting enough exercise. In addition to these common causes of constipation, other causes in people with cancer include:
| Medicines. Chemotherapy, opioids, antidepressants, antacids, and diuretics can cause constipation by affecting the nerves and muscles in the digestive tract, slowing down bowel movements. |
| Changes in your bathroom habits. You may have little or no privacy and need help to get to the bathroom. |
| Limited mobility. Long periods of inactivity due to cancer can cause constipation. |
| Bowel disorders. This includes disorders such as irritable bowel and diverticulitis. |
| Muscle and nerve disorders. A spinal cord injury or pressure on the spinal cord from a tumor can cause constipation. |
| Metabolic changes. Some cancers can affect your appetite and ability to absorb, store, and use nutrients. |
| Depression. Depression can lead to lower levels of activity and changes in bodily functions. Constipation can also be a side effect of medicines that treat depression. |
Assessment of constipation includes a health history, physical exam, and other tests.
The following tests and procedures may be done to help diagnose constipation:
- Health history: A discussion with your doctor about your bowel habits, including frequency, stool consistency, and whether you are experiencing symptoms such as pain, bloating, or nausea when you are constipated. The doctor will also ask about your diet, fluid intake, and medicines you are taking and whether there have been recent changes in any of these areas. For people who have colostomies, care of the colostomy will be discussed.
- Physical exam: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. The doctor will check the abdomen to see if it is swollen, listen for bowel sounds, and feel for painful areas in the abdomen.
If the cause of the constipation isn't clear from the health history and physical exam, your doctor may order more tests to find out if another problem is causing the constipation:
- Digital rectal exam (DRE): An exam of the rectum. The doctor or nurse inserts a lubricated, gloved finger into the lower part of the rectum to feel for lumps or anything else that seems unusual. In women, the vagina may also be examined.
- Fecal occult blood test: A test to check stool for blood that can only be seen with a microscope. Small samples of stool are placed on special cards and returned to the doctor or laboratory for testing.

A guaiac fecal occult blood test (FOBT) checks for occult (hidden) blood in the stool. Small samples of stool are placed on a special card and returned to a doctor or laboratory for testing.
- Abdominal x-ray: An x-ray of the organs inside the abdomen. An x-ray is a type of high-energy radiation that can go through the body and onto film, making a picture of areas inside the body.
- Sigmoidoscopy: A procedure to look inside the rectum and sigmoid (lower) colon for polyps, abnormal areas, or cancer. A sigmoidoscope is inserted through the rectum into the sigmoid colon. A sigmoidoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
- Colonoscopy: A procedure to look inside the rectum and colon for polyps, abnormal areas, or cancer. A colonoscope is inserted through the rectum into the colon. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
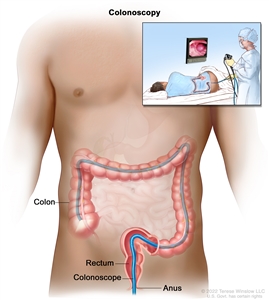
Colonoscopy. A thin, lighted tube is inserted through the anus and rectum and into the colon to look for abnormal areas.
It is important to prevent and treat constipation to avoid serious problems.
The health care team will talk to you about ways to prevent and treat constipation. Constipation can be uncomfortable and cause distress. If left untreated, constipation may lead to fecal impaction. This is a serious condition in which stool will not pass out of the colon or rectum. It's important to treat constipation to prevent fecal impaction.
Prevention and treatment of constipation are not the same for every person. Keep track of how often you have a bowel movement and do the following to prevent and treat constipation:
- Drink more fluid each day unless you have a medical condition that restricts fluid intake.
- Get regular exercise. People who cannot walk may do abdominal exercises in bed or move from the bed to a chair.
- Increase the amount of fiber in the diet. It's important to drink more fluids when eating more high-fiber foods, to avoid making constipation worse. People who have had a small or large intestinal obstruction or have had intestinal surgery (for example, a colostomy) should not eat a high-fiber diet.
- Drink a warm or hot drink about one half-hour before the usual time for a bowel movement.
- Find privacy and quiet when it is time for a bowel movement.
- Use the toilet or a bedside commode instead of a bedpan.
- People who take opioids may need to start taking laxatives right away to prevent constipation. Other drugs may be given to prevent constipation.
People at risk of bleeding or infection should talk with their doctor before using suppositories or enemas.
Fecal Impaction
Fecal impaction is a severe form of constipation in which dry, hard stool cannot pass out of the colon or rectum.
Fecal impaction is dry stool that cannot pass out of the body. Constipation that is not treated can lead to fecal impaction. For this reason, the causes of fecal impaction are the same as those of constipation. To learn more, see the section on causes of constipation.
Fecal impaction and constipation share similar symptoms, but fecal impaction may cause other severe symptoms, such as breathing problems, dizziness, or low blood pressure.
Symptoms of fecal impaction include:
- being unable to have a bowel movement
- having to push harder to have a bowel movement of small amounts of hard, dry stool
- having fewer than the usual number of bowel movements
- having a swollen abdomen
- having pain in the back or abdomen
- urinating more or less often than usual, or being unable to urinate
- having breathing problems
- having a rapid heartbeat or chest pain
- dizziness or low blood pressure
- having sudden, explosive diarrhea (as stool moves around the impaction)
- leaking stool when coughing
- nausea and vomiting
- dehydration
- being confused and losing a sense of time and place, with a rapid heartbeat, sweating, fever, and high or low blood pressure
It's important to talk with your health care provider if you have these symptoms.
Assessment of constipation includes a health history, physical exam, and other tests.
The following tests and procedures may be done to help diagnose fecal impaction:
- Health history: A discussion with your doctor about your bowel habits, including frequency, stool consistency, and whether you are experiencing symptoms such as pain, bloating, or nausea when you are constipated. The doctor will also ask about your diet, fluid intake, and medicines you are taking and whether there have been recent changes in any of these areas.
- Physical exam: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. The doctor will check the abdomen to see if it is swollen, listen for bowel sounds, and feel for painful areas in the abdomen.
- Abdominal x-rays: An x-ray of the organs inside the abdomen. An x-ray is a type of high energy radiation that can go through the body and onto film, making a picture of areas inside the body to check for fecal impaction.
- Digital rectal exam (DRE): An exam of the rectum. The doctor or nurse inserts a lubricated, gloved finger into the lower part of the rectum to feel for a fecal impaction, lumps, or anything else that seems unusual.
- Sigmoidoscopy: A procedure to look inside the rectum and sigmoid (lower) colon for a fecal impaction, polyps, abnormal areas, or cancer. A sigmoidoscope is inserted through the rectum into the sigmoid colon. A sigmoidoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
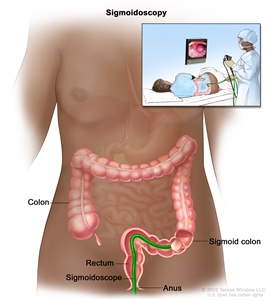
Sigmoidoscopy. A thin, lighted tube is inserted through the anus and rectum and into the lower part of the colon to look for abnormal areas.
Fecal impaction is usually treated with an enema.
The main treatment for impaction is to moisten and soften the stool so it can be removed or passed out of the body. This is usually done with an enema. Enemas are given only as prescribed by the doctor to reduce the risk of bleeding or infection for patients with low blood counts and because too many enemas can damage the intestine. Some people may need to have stool manually removed from the rectum after it is softened.
Bowel Obstruction
A bowel obstruction is a blockage of the small or large intestine by something other than fecal impaction.
A bowel obstruction (blockage) may be caused by a twist in an intestine, a hernia, inflammation, scar tissue from surgery, or cancer. The obstruction keeps the stool from moving through the small or large intestines. The intestine may be partly or completely blocked and can sometimes be blocked in two places.
A bowel obstruction may cause decreased blood flow to an area of the intestines. Blood flow needs to be corrected or the affected tissue may die.
Cancers in the stomach, colon, and ovary can spread to the abdomen and cause an obstruction. People with these cancers or those who have had surgery or radiation therapy to the abdomen have a higher risk of a bowel obstruction. Bowel obstructions are most common during the advanced stages of cancer.
A bowel obstruction can cause pain.
The following may be symptoms of a bowel obstruction:
- abdominal pain or cramps
- swelling in the abdomen
- constipation
- diarrhea
- nausea or vomiting
- problems passing gas
- loss of appetite
It's important to talk with your health care provider if you have these symptoms.
Assessment of a bowel obstruction includes a physical exam and imaging tests.
The following tests and procedures may be done to diagnose a bowel obstruction:
- Physical exam: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual.
- Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for the following:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
- Electrolyte panel: A blood test that measures the levels of electrolytes, such as sodium, potassium, and chloride.
- Urinalysis: A test to check the color of urine and its contents, such as sugar, protein, red blood cells, and white blood cells.
- CT scan (CAT scan): This procedure uses a computer linked to an x-ray machine to make a series of detailed pictures of areas inside the body, such as the abdomen, taken from different angles. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- Abdominal x-ray: An x-ray of the organs inside the abdomen. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- Barium enema: A series of x-rays of the lower gastrointestinal tract. A liquid that contains barium (a silver-white metallic compound) is put into the rectum. The barium coats the lower gastrointestinal tract and x-rays are taken. This procedure is also called a lower GI series. This test may show what part of the intestine is blocked.
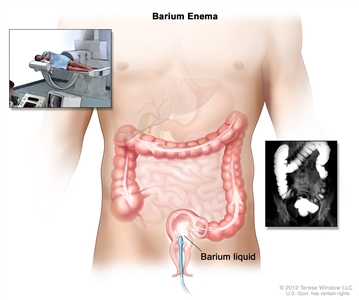
Barium enema procedure. The patient lies on an x-ray table. Barium liquid is put into the rectum and flows through the colon. X-rays are taken to look for abnormal areas.
Treatment for acute bowel obstruction may include surgery.
Acute bowel obstructions occur suddenly and can be treated. Treatment may include the following:
- Fluid replacement therapy: A treatment to get the fluids in the body back to normal amounts. Intravenous (IV) fluids may be given and medicines may be prescribed.
- Electrolyte correction: A treatment to get the right amounts of chemicals in the blood, such as sodium, potassium, and chloride. Fluids with electrolytes may be given by infusion.
- Blood transfusion: A procedure in which a person is given an infusion of whole blood or parts of blood.
- Bowel rest: Food and sometimes fluid are held to give the intestines time to heal.
- Nasogastric or colorectal tube: A nasogastric tube is inserted through the nose and esophagus into the stomach. A colorectal tube is inserted through the rectum into the colon. This is done to decrease swelling, remove fluid and gas buildup, and relieve pressure.
- Stents: A metal tube inserted into the intestine to open the area that is blocked to relieve symptoms caused by the blockage.
- Surgery: Surgery to relieve the obstruction may be done if it causes serious symptoms that are not relieved by other treatments.
People with symptoms that keep getting worse will have follow-up exams to check for signs and symptoms of shock and to make sure the obstruction isn't getting worse.
Treatment of a chronic, malignant bowel obstruction may include surgery to improve quality of life.
Chronic, malignant bowel obstructions may worsen over time. People with advanced cancer may have chronic bowel obstructions that cannot be removed with surgery. The intestine may be blocked or narrowed in more than one place or the tumor may be too large to remove completely. Treatments include the following:
- Surgery: The obstruction is removed to relieve pain and improve the patient's quality of life.
- Stent: A metal tube inserted into the intestine to open the area that is blocked to relieve symptoms and improve the patient's quality of life.
- Gastrostomy tube: A tube inserted through the wall of the abdomen directly into the stomach. The gastrostomy tube can be attached to a drainage bag with a valve. When the valve is open the built-up fluid and air can leave the stomach to relieve symptoms caused by the obstruction. People may also be able to eat or drink by mouth because the food drains directly into the bag. This gives the person the experience of tasting the food and keeping the mouth moist. Solid food is avoided because it may block the tubing to the drainage bag. If the person has an obstruction that is not completely blocking the intestine, they may also use the gastrostomy tube to pour medications directly into the stomach.
- Medicines: Injections or infusions of medicines for pain, nausea and vomiting, and/or to make the intestines empty. This may be prescribed for people who cannot have surgery or be helped with a stent or gastrostomy tube.
Diarrhea
Diarrhea is frequent, loose, and watery bowel movements.
Acute diarrhea is three or more loose or watery bowel movements in one day. Acute diarrhea may last more than 4 days but less than 2 weeks. Frequent, watery stools that last for more than 2 months is called chronic diarrhea. Diarrhea can occur at any time during cancer treatment. It can be physically and emotionally stressful for people with cancer.
Cancer treatment is the most common cause of diarrhea in people with cancer.
Causes of diarrhea in people with cancer include the following:
- Cancer treatments, such as chemotherapy, targeted therapy, immunotherapy, radiation therapy, bone marrow transplant, and surgery.
- Some chemotherapy and targeted therapy drugs cause diarrhea by changing how nutrients are broken down and absorbed in the small intestine.
- Immunotherapy is a type of cancer treatment that helps your immune system fight cancer. As it attacks cancer cells, it also attacks healthy cells and tissues. This may result in diarrhea.
- Radiation therapy to the abdomen and pelvis can cause inflammation of the bowel. Diarrhea may last up to 8 to 12 weeks after treatment or may not happen for months or years. People who are having radiation therapy and chemotherapy often have severe diarrhea.
- People who have a donor bone marrow transplant may develop graft-versus-host disease (GVHD). Stomach and intestinal symptoms of GVHD include nausea and vomiting, severe abdominal pain and cramps, and watery, green diarrhea. Symptoms may show up 1 week to 3 months after the transplant.
- Surgery on the stomach or intestines.
- The cancer itself.
- Stress and anxiety from being diagnosed with cancer and having cancer treatment.
- Medical conditions and diseases other than cancer.
- Infections.
- Antibiotic therapy for certain infections. Antibiotic therapy can irritate the lining of the bowel and cause diarrhea that often does not get better with treatment.
- Tubefeeding.
- Fecal impaction in which the stool leaks around the blockage.
- Certain foods such as milk products, fruits, vegetables, and foods that are high in fiber or fat.
Assessment of diarrhea includes a health history, physical exam, and lab tests.
Diarrhea can cause life-threatening complications in people with cancer. It is important to find out the cause so treatment can begin as soon as possible.
The following tests and procedures may be done to diagnose diarrhea and help plan treatment:
- Health history: A discussion with your doctor about your urine habits and bowel habits, including frequency, stool consistency, and whether you are experiencing symptoms such as dizziness, drowsiness, pain, nausea and vomiting, or fever. The doctor will also ask about your recent diet and fluid intake, recent travels, and medicines you are taking and how often.
- Physical exam: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. The doctor will check the abdomen for painful areas and listen for bowel sounds.
- Digital rectal exam (DRE): An exam of the rectum. The doctor or nurse inserts a lubricated, gloved finger into the lower part of the rectum to feel for lumps or anything else that seems unusual. The exam will check for signs of fecal impaction. Stool may be collected for laboratory tests.
- Fecal occult blood test: A test to check stool for blood that can only be seen with a microscope. Small samples of stool are placed on special cards and returned to the doctor or laboratory for testing.
- Stool tests: Laboratory tests to check the water and sodium levels in stool, and to find substances that may be causing diarrhea. Stool is also checked for bacterial, fungal, or viral infections.
- Complete blood count (CBC): A procedure in which a sample of blood is drawn and checked for the following:
- the number of red blood cells, white blood cells, and platelets
- the amount of hemoglobin (the protein that carries oxygen) in the red blood cells
- the portion of the blood sample made up of red blood cells
- Electrolyte panel: A blood test that measures the levels of electrolytes, such as sodium, potassium, and chloride.
- Urinalysis: A test to check the color of urine and its contents, such as sugar, protein, red blood cells, and white blood cells.
- Abdominal x-ray: An x-ray of the organs inside the abdomen. An x-ray is a type of high-energy radiation that can go through the body and onto film, making a picture of areas inside the body. Abdominal x-rays may also be done to look for a bowel obstruction or other problems.
Treatment of diarrhea depends on what is causing it.
Treatment depends on the cause of the diarrhea. The doctor may make changes to your medicines, diet, and/or fluids. Treatment of diarrhea may include the following:
- A change in the use of laxatives may be needed.
- Medicine to treat diarrhea may be prescribed to slow down the intestines, decrease fluid secreted by the intestines, and help nutrients be absorbed.
- Diarrhea caused by cancer treatment may be treated by changes in diet. Eat small frequent meals and avoid the following foods:
- milk and dairy products
- spicy foods
- alcohol
- foods and drinks that have caffeine
- certain fruit juices
- foods and drinks that cause gas
- foods high in fiber or fat
- Drink more clear liquids to help stay hydrated. These include water, sports drinks, broth, weak decaffeinated tea, caffeine-free soft drinks, clear juices, and gelatin. For severe diarrhea, the person may need intravenous (IV) fluids or other forms of IV nutrition.
- Diarrhea caused by graft-versus-host-disease (GVHD) is often treated with a special diet. Some people may need long-term treatment and diet management.
- Probiotics may be suggested. Probiotics are live microorganisms used as a dietary supplement to help with digestion and normal bowel function. Research on the use of Lactobacillus acidophilus and Bifidobacterium has reported benefits in treating diarrhea.
- People who have diarrhea with other symptoms may need fluids and medicine given by IV.
Radiation Enteritis
Radiation enteritis is inflammation of the intestine caused by radiation therapy.
The small and large intestine are sensitive to radiation. Radiation therapy given to kill cancer cells in the abdomen and pelvis affects normal cells in the lining of the intestines. Radiation therapy stops the growth of cancer cells and other fast-growing cells. Since normal cells in the lining of the intestines grow quickly, radiation treatment to that area can stop those cells from growing. This makes it hard for tissue to repair itself. As cells die and are not replaced, gastrointestinal problems occur over the next few days and weeks.
Radiation enteritis is a condition in which the lining of the intestine becomes swollen and inflamed during or after radiation therapy to the abdomen, pelvis, or rectum. The larger the dose of radiation, the more damage may be done to normal tissue.
Radiation enteritis may be acute or chronic:
- Acute radiation enteritis occurs during radiation therapy or within three months after finishing radiation therapy.
- Chronic radiation enteritis may appear months after radiation therapy ends.
The total dose of radiation and other factors affect the risk of radiation enteritis.
The amount of time the enteritis lasts and how severe it is depend on the following:
- the type and total dose of radiation received
- the amount of normal intestine treated
- the tumor size and how much it has spread
- if chemotherapy was given at the same time as the radiation therapy
- if the person has had surgery to the abdomen or pelvis
- if the person has high blood pressure, diabetes, a smoking history, or poor nutrition
About 10% to 20% of people treated with radiation to the abdomen will have chronic problems.
Acute and chronic radiation enteritis have similar symptoms.
People with acute radiation enteritis may have the following symptoms:
- nausea
- vomiting
- abdominal cramps
- frequent urges to have a bowel movement
- rectal pain, bleeding, or mucus in the stool
- watery diarrhea
- feeling very tired
Symptoms of acute enteritis usually go away 2 to 3 weeks after treatment ends.
Symptoms of chronic radiation enteritis usually appear 6 to 18 months after radiation therapy ends. It can be hard to diagnose. The doctor will first check to see if the symptoms are being caused by a recurrent tumor in the intestine. The doctor will also need to know the person's full history of radiation treatments.
People with chronic radiation enteritis may have the following signs and symptoms:
- abdominal pain
- bloody diarrhea
- greasy and fatty stools
- weight loss
- nausea
- vomiting
It's important to talk with your health care provider if you have these symptoms.
Assessment of radiation enteritis includes a physical exam and health history.
A doctor will do a physical exam and ask questions about the following:
- usual pattern of bowel movements
- pattern of diarrhea:
- when it started
- how long it has lasted
- how often it occurs
- amount and type of stools
- other symptoms with the diarrhea (such as gas, cramping, bloating, urgency, bleeding, and rectal soreness)
- nutrition health:
- height and weight
- usual eating habits
- changes in eating habits
- amount of fiber in the diet
- signs of dehydration (such as poor skin tone, increased weakness, or feeling very tired)
- stress levels and ability to cope
- changes in lifestyle caused by the enteritis
Treatment of acute radiation enteritis includes treating the symptoms.
The symptoms of radiation enteritis usually get better with treatment, but if symptoms get worse, then cancer treatment may have to be stopped for a while.
Treatment of acute radiation enteritis or the symptoms may include:
- anti-inflammatory medicines that improve the flow of blood through the body
- antibiotics
- steroids
- medicines to stop diarrhea and to lower cholesterol in the blood
- vitamin E
- probiotic
- diet changes
- Intestines damaged by radiation therapy may not make enough of certain enzymes needed for digestion, especially lactase. Lactase is needed to digest lactose, which is found in milk and milk products. A lactose-free, low-fat, and low-fiber diet may help control symptoms of acute enteritis. Foods to avoid:
- milk and some milk products
- whole-bran bread and cereal
- nuts, seeds, and coconut
- fried, greasy, or fatty foods
- fresh and dried fruit and some fruit juices (such as prune juice)
- raw vegetables
- rich pastries
- popcorn, potato chips, and pretzels
- strong spices and herbs
- chocolate, coffee, tea, and soft drinks with caffeine
- alcohol and tobacco
- Foods to choose:
- fish, poultry, and meat that are broiled or roasted
- bananas
- applesauce and peeled apples
- apple and grape juices
- white bread and toast
- pasta
- baked, boiled, or mashed potatoes
- cooked vegetables that are mild, such as asparagus tips, green and waxed beans, carrots, spinach, and squash
- mild processed cheese, which may not cause problems because the lactose is removed when it is made
- buttermilk, yogurt, and lactose-free milkshake supplements, such as Ensure
- eggs
- smooth peanut butter
- Helpful hints:
- Eat food at room temperature.
- Drink about 12 eight-ounce glasses of fluid a day.
- Let sodas lose their fizz before drinking them.
- Add nutmeg to food. This helps slow down movement of digested food in the intestines.
- Start a low-fiber diet on the first day of radiation therapy.
Treatment of chronic radiation enteritis may include the same treatments for acute radiation enteritis.
Treatment of chronic radiation enteritis may include the following:
- same treatments as for acute radiation enteritis symptoms
- surgery may be needed to control symptoms in some patients. Two types of surgery may be used:
- Intestinal bypass: A procedure in which the doctor creates a new pathway for the flow of intestinal contents around the damaged tissue.
- Total intestinal resection: Surgery to completely remove the intestines.
Doctors look at the person's general health and the amount of damaged tissue before deciding if surgery will be needed. Healing after surgery is often slow and long-term tubefeeding may be needed. Even after surgery, many people still have symptoms.
Current Clinical Trials
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Gastrointestinal Complications
For more information from the National Cancer Institute about constipation or diarrhea, see the following:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government's center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the causes and treatment of gastrointestinal complications, including constipation, impaction, bowel obstruction, diarrhea, and radiation enteritis. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Supportive and Palliative Care Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as "NCI's PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary]."
The best way to cite this PDQ summary is:
PDQ® Supportive and Palliative Care Editorial Board. PDQ Gastrointestinal Complications. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: https://www.cancer.gov/about-cancer/treatment/side-effects/constipation/GI-complications-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389438]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website's E-mail Us.
Last Revised: 2024-01-05
If you want to know more about cancer and how it is treated, or if you wish to know about clinical trials for your type of cancer, you can call the NCI's Cancer Information Service at 1-800-422-6237, toll free. A trained information specialist can talk with you and answer your questions.