Condition Basics
What are peptic ulcers, and what causes them?
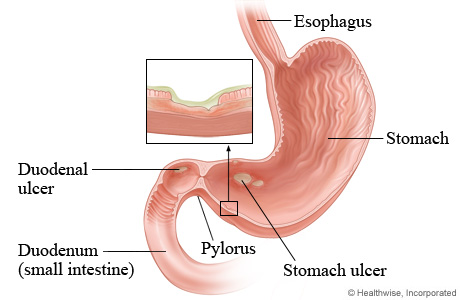
Peptic ulcers are sores in the inner lining of the stomach or upper small intestine. They form when the digestive juices produced by the stomach erode or eat away the lining of the digestive tract. Peptic ulcers may form in the lining of the stomach (gastric ulcers) or just below the stomach, at the start of the small intestine (duodenal ulcers).
The most common causes of peptic ulcers are infection with Helicobacter pylori (H. pylori) bacteria and long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include aspirin, ibuprofen (Advil or Motrin), and naproxen (Aleve).
What are the symptoms?
Symptoms of a peptic ulcer can include a burning, aching, or gnawing pain between the belly button and the breastbone, and belly pain that is temporarily relieved by taking an antacid. Symptoms can also include back pain, loss of appetite, bloating, nausea, and vomiting. Some people have no symptoms.
How are they diagnosed?
Your doctor will ask about your symptoms and do a physical exam. Your doctor may do some simple tests (using your blood, breath, or stool) to look for signs of H. pylori infection. You may have an endoscopy to check the inside of your esophagus, stomach, and small intestine.
How are peptic ulcers treated?
To treat peptic ulcers, most people take medicines that reduce acid in the stomach. If you have an H. pylori infection, you'll also take antibiotics. You can help your ulcer heal by quitting smoking and avoiding alcohol. Using medicines such as aspirin, ibuprofen, or naproxen may increase the chance of your ulcer returning.
Cause
The most common causes of peptic ulcers are infection with Helicobacter pylori (H. pylori) bacteria and use of nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include aspirin, ibuprofen (Advil or Motrin), and naproxen (Aleve). H. pylori and NSAIDs break down the protective mucus layer in the stomach or intestine.
Learn more
What Increases Your Risk
Doing the following things can increase your chance of getting a peptic ulcer. They may also slow the healing of an ulcer you already have.
- Taking nonsteroidal anti-inflammatory drugs (NSAIDs). These include aspirin, ibuprofen (Advil or Motrin), and naproxen (Aleve).
- Smoking.
- Drinking too much alcohol.
Some things that you can't control may increase your risk of getting an ulcer.
- A Helicobacter pylori (H. pylori) bacterial infection. This is the most common cause of ulcers.
- Physical stress caused by a serious illness or injury. Examples are a major trauma, surgery, or the need to be on a ventilator to assist breathing.
- Hypersecretory condition. With this, your stomach produces too much acid.
- A personal or family history of ulcers.
Symptoms
Common symptoms of a peptic ulcer include:
- A burning, aching, or gnawing pain between the belly button (navel) and the breastbone. Some people also have back pain. The pain can last from a few minutes to a few hours. It may come and go for weeks.
- Pain that usually goes away for a while after you take an antacid or acid reducer.
- Loss of appetite and weight loss.
- Bloating or nausea after eating.
Less common symptoms include:
- Vomiting.
- Vomiting blood or material that looks like coffee grounds.
- Passing black stools that look like tar, or stools that contain dark red blood.
Different people have different symptoms.
Some ulcers don't cause symptoms. These are known as silent ulcers.
What Happens
The symptoms of peptic ulcers, such as belly pain, may come and go. Some ulcers will heal by themselves. But even with treatment, ulcers sometimes come back. They may cause problems like bleeding or perforation. That's why it's important to treat an ulcer, even if you don't have any symptoms.
Complications
A peptic ulcer may cause problems such as:
- Bleeding.
-
Peptic ulcers sometimes bleed.
- Sometimes an ulcer may involve just the surface lining of the digestive tract. The person may then have a slow but constant loss of blood into the digestive tract. Over time, this may cause anemia.
- If ulcers become larger and go deeper into the digestive tract lining, they may damage large blood vessels. This can result in sudden, serious bleeding into the intestinal tract.
- Perforation.
-
Perforation occurs when an ulcer eats through the wall of the stomach or intestine into the belly cavity.
- When perforation happens, partly digested food, bacteria, and enzymes from the digestive tract may spill into the belly cavity. This causes inflammation and infection (peritonitis).
- Peritonitis usually causes sudden and severe pain. In most cases, treatment requires an urgent stay in the hospital and surgery.
When to Call a Doctor
If you have been diagnosed with a peptic ulcer, call 911 or other emergency services immediately if you have:
- Symptoms that could be a sign of a heart attack.
- Sudden, severe, continuous belly pain or vomiting.
- Vomit or stool that has a large amount of bright red blood.
Call your doctor now if you have:
- Dizziness or lightheadedness, or you feel like you may faint.
- Blood in your vomit or something that looks like coffee grounds (partially digested blood) in your vomit.
- Stools that are black or that look like tar, or stools that contain dark red or maroon blood.
Call your doctor if you have been diagnosed with a peptic ulcer and:
- Your symptoms continue or get worse after 10 to 14 days of treatment.
- You start to lose weight without trying.
- You are vomiting.
- You have new belly pain or belly pain that doesn't go away.
Watchful waiting
If you've been diagnosed with a peptic ulcer and medical treatment isn't helping, call your doctor. Waiting until your symptoms get worse can be serious.
If you don't know if you have a peptic ulcer and you don't have any of the emergency symptoms listed above, you may try taking an antacid or nonprescription acid reducer and other home treatment, such as making changes to your diet.
- If your symptoms don't get better after 10 to 14 days, call your doctor.
- If your symptoms go away after you take antacids or acid reducers and try home treatment, but then the symptoms come back, call your doctor.
Exams and Tests
Your doctor will ask you questions about your symptoms and your general health. The doctor will do a physical exam.
Your doctor may test you for an H. pylori infection. This is done using your breath, blood, or stool.
The only way for you and your doctor to know for sure if you have an ulcer is to do an endoscopy. An endoscopy allows the doctor to look inside your esophagus, stomach, and small intestine. It's done to look for an ulcer and to test for an H. pylori infection.
You may get other tests to find problems that are caused by peptic ulcers. Tests may include blood tests or X-rays.
Learn more
Watch
Treatment Overview
To treat peptic ulcers, most people need to take medicines that reduce the amount of acid in the stomach. If you have an H. pylori infection, you will also need to take antibiotics.
You can help speed the healing of your ulcer and help prevent it from coming back if you quit smoking and avoid alcohol. If you keep using medicines such as aspirin, ibuprofen, or naproxen, you may increase the chance of your ulcer coming back.
Surgery is rarely used to treat an ulcer. But if your ulcer doesn't heal, or if you have life-threatening complications, you may need surgery.
Ignoring symptoms of an ulcer isn't a good idea. An ulcer needs to be treated. While symptoms can go away for a short time, you may still have an ulcer. Left untreated, an ulcer can cause life-threatening problems. Even with treatment, some ulcers may come back and may need more treatment.
Learn more
Self-Care
- Be safe with medicines. Take your medicines exactly as prescribed. Call your doctor if you think you are having a problem with your medicine.
- Do not take aspirin or other NSAIDs such as ibuprofen (Advil or Motrin) or naproxen (Aleve). Ask your doctor what you can take for pain.
- If you smoke, try to quit. Smoking can make ulcers worse. If you need help quitting, talk to your doctor about stop-smoking programs and medicines. These can increase your chances of quitting for good.
- Avoid drinking alcohol as much as you can.
- Eat a balanced diet of small, frequent meals. See a dietitian if you need help planning your meals. Avoid foods that make your symptoms worse.
Learn more
Watch
Medicines
Peptic ulcers are treated with medicines. You can get some of these medicines over the counter. Medicines can do different things. They can:
- Reduce stomach acid.
- Medicines that reduce the amount of stomach acid include:
-
- Antacids, such as Tums.
- Acid reducers, such as:
- H2 blockers like famotidine (Pepcid).
- Proton pump inhibitors (PPI) like omeprazole (Prilosec).
- Treat an H. pylori infection.
- If you have an H. pylori infection, you usually get antibiotics and a PPI. Sometimes you will also get a bismuth medicine.
- Protect the stomach lining.
- If your ulcer is from use of aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), you usually get medicines that protect the stomach lining from damage. These include:
- Acid reducers, such as H2 blockers like cimetidine (Tagamet).
- PPIs like omeprazole (Prilosec).
Learn more
Credits
Current as of: October 19, 2023